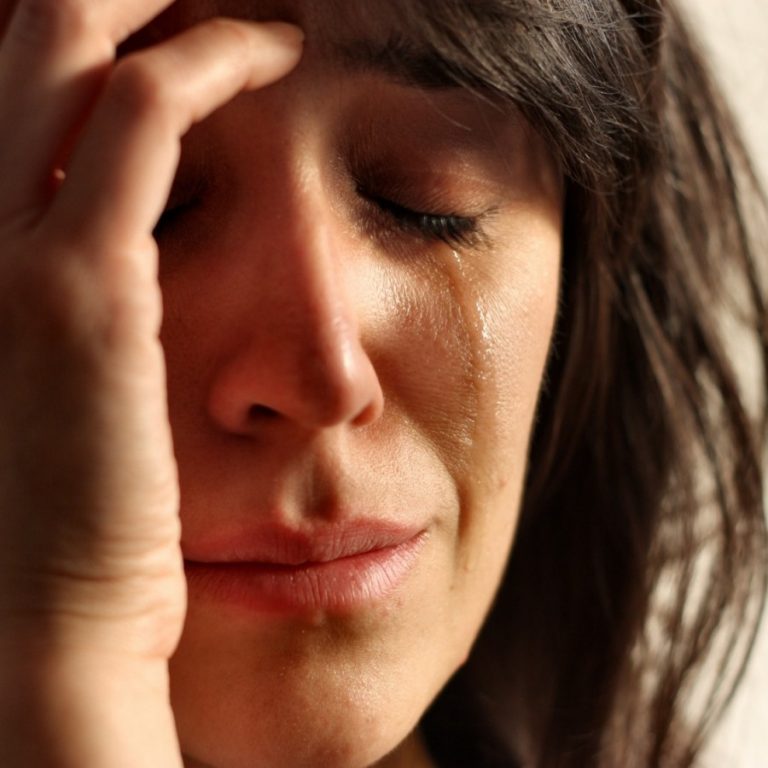
Rise In Mental Illness Linked To Unhealthy Diets, Say Studies
Changes in diet over the past 50 years appear to be an important factor behind a significant rise in mental ill health in the UK, say two reports published today.
The Mental Health Foundation says scientific studies have clearly linked attention deficit disorder, depression, Alzheimer’s disease and schizophrenia to junk food and the absence of essential fats, vitamins and minerals in industrialised diets. A further report, Changing Diets, Changing Minds, is also published today by Sustain, the organisation that campaigns for better food. It warns that the NHS bill for mental illness, at almost £100bn a year, will continue to rise unless the government focuses on diet and the brain in its food, farming, education and environment policies.
“Food can have an immediate and lasting effect on mental health and behaviour because of the way it affects the structure and function of the brain,” Sustain’s report says. Its chairman, Tim Lang, said: “Mental health has been completely neglected by those working on food policy. If we don’t address it and change the way we farm and fish, we may lose the means to prevent much diet-related ill health.”
Both reports, which have been produced collaboratively, outline the growing scientific evidence linking poor diet to problems of behaviour and mood. Rates of depression have been shown to be higher in countries with low intakes of fish, for example. Lack of folic acid, omega-3 fatty acids, selenium and the amino acid tryptophan are thought to play an important role in the illness. Deficiencies of essential fats and antioxidant vitamins are also thought to be a contributory factor in schizophrenia.
A pioneering nutrition and mental health programme, thought to be the only one of its kind in Britain, was carried out at Rotherham, South Yorkshire. According to Caroline Stokes, its research nutritionist, the mental health patients she saw generally had the poorest diets she had ever come across. “They are eating lots of convenience foods, snacks, takeaways, chocolate bars, crisps. It’s very common for clients to be drinking a litre or two of cola a day. They get lots of sugar but a lot of them are eating only one portion of fruit or vegetable a day, if that.”


The therapy includes omega-3 fatty acids and multivitamins, with advice on cutting out junk food and replacing it with oily fish, leafy vegetables for folic acid, Brazil nuts for selenium, and food providing tryptophan.
Some patients who resist treatment with drugs accept nutritional therapy and most have reported an improvement in mood and energy. Ms Stokes said: “Within the first month there’s been a significant reduction in depression. We’ve had letters from [the patients’] psychiatrists saying they can see a huge difference.”
One sufferer who benefited from a dietary change was James McLean, who was at university when first diagnosed with bipolar disorder (manic depression). After he had been sectioned repeatedly, his father read about the role of nutrition in mental health. The pair went privately to the Brain Bio Centre, in London, where Mr McLean’s nutrient levels were checked; he was allergic to gluten and yeast and was given supplements, including vitamin B and essential fatty acids.
“I’d been eating lots of intense carbohydrate foods … because they were cheap, and very little fruit or vegetables,” Mr McLean said. Now, he excludes wheat from his diet too. He added: “I have more energy and confidence, I sleep better, and I came off the anti-psychotic drugs, although I still take mood stabilising ones.”
Andrew McCulloch, chief executive of the Mental Health Foundation, acknowledged that mental illness results from a complex interplay of biological, social, psychological and environmental factors, but thought diet should be an everyday component of mental health care. “It costs £1,000 a week to keep someone in a psychiatric hospital. How much does good food cost? We need mentally healthy school meals, and mentally healthy hospital foods,” he said.
Best choices and worst:
Good for the brain:
Vegetables, especially leafy
Seeds and nuts
Fruit
Whole grains
Wheatgerm
Organic eggs
Organic farmed or wild fish, especially fatty fish
Bad for the brain:
Deep fried junk foods
Refined processed foods
Pesticides
Alcohol
Sugar
Tea and coffee
Some additives
Felicity Lawrence
Monday January 16, 2006
The Guardian