Obesity Help And Microflora


In the 30-plus years that Richard Atkinson has been studying obesity, he has always maintained that overeating doesn’t really explain it all. His epiphany came early in his career, when he was a medical fellow at U.C.L.A. engaged in a study of people who weighed more than 300 pounds and had come in for obesity surgery. “The general thought at the time was that fat people ate too much,” Atkinson, now at Virginia Commonwealth University, told me recently. “And we documented that fat people do eat too much — our subjects ate an average of 6,700 calories a day. But what was so impressive to me was the fact that not all fat people eat too much.”
One of Atkinson’s most memorable patients was Janet S., a bright, funny 25-year-old who weighed 348 pounds when she finally made her way to U.C.L.A. in 1975. In exchange for agreeing to be hospitalized for three months so scientists could study them, Janet and the other obese research subjects (30 in all) each received a free intestinal bypass. During the three months of presurgical study, the dietitian on the research team calculated how many calories it should take for a 5-foot-6-inch woman like Janet to maintain a weight of 348. They fed her exactly that many calories — no more, no less. She dutifully ate what she was told, and she gained 12 pounds in two weeks — almost a pound a day.
“I don’t think I’d ever gained that much weight that quickly,” recalled Janet, who asked me not to use her full name because she didn’t want people to know how fat she had once been. The doctors accused her of sneaking snacks into the hospital. “But I told them, ‘I’m gaining weight because you’re feeding me a tremendous amount of food!’ ”
The experience with Janet was an early inkling that traditional ideas about obesity were incomplete. Researchers and public-health officials have long understood that to maintain a given weight, energy in (calories consumed) must equal energy out (calories expended). But then they learned that genes were important, too, and that for some people, like Janet, this formula was tilted in a direction that led to weight gain. Since the discovery of the first obesity gene in 1994, scientists have found about 50 genes involved in obesity. Some of them determine how individuals lay down fat and metabolize energy stores. Others regulate how much people want to eat in the first place, how they know when they’ve had enough and how likely they are to use up calories through activities ranging from fidgeting to running marathons. People like Janet, who can get fat on very little fuel, may be genetically programmed to survive in harsher environments. When the human species got its start, it was an advantage to be efficient. Today, when food is plentiful, it is a hazard.
But even as our understanding of genes and behavior has become more refined, some cases still boggle the mind, like identical twins who eat roughly the same and yet have vastly different weights. Now a third wave of obesity researchers are looking for explanations that don’t fall into the relatively easy ones of genetics, overeating or lack of exercise. They are investigating what might seem to be the unlikeliest of culprits: the microorganisms we encounter every day.
One year ago, the idea that microbes might cause obesity gained a foothold when the Pennington Biomedical Research Center in Louisiana created the nation’s first department of viruses and obesity. It is headed by Nikhil Dhurandhar, a physician who invented the term “infectobesity” to describe the emerging field. Dhurandhar’s particular interest is in the relationship between obesity and a common virus, the adenovirus. Other scientists, led by a group of microbiologists at Washington University in St. Louis, are looking at the actions of the trillions of microbes that live in everyone’s gut, to see whether certain intestinal microbes may be making their hosts fat.
If microbes help explain even a small proportion of obesity, that could shed light on a condition that plagues millions of Americans. Today 30.5 percent of the American public is obese; that is, nearly a third of Americans have a body-mass index over 30 (which for someone of Janet’s height is 186 pounds). The Department of Health and Human Services says obesity may account for 300,000 deaths a year, making it the second-most-common preventable cause of death after cigarette smoking. It’s been linked to various diseases: diabetes, high blood pressure, heart disease, gallbladder disease, sleep apnea, osteoarthritis and some cancers. “Individuals who are obese,” the department states on its Web site, “have a 50 to 100 percent increased risk of premature death from all causes, compared to individuals with a healthy weight.”
If microbes do turn out to be relevant, at least in some cases of obesity, it could change the way the public thinks about being fat. Along with the continuing research on the genetics of obesity, the study of other biological factors could help mitigate the negative stereotypes of fat people as slothful and gluttonous and somehow less virtuous than thin people. There is, of course, the risk of overemphasizing how potent the biological forces are that make some people prone to gaining weight. Biology sets the context, and that is critical, but obesity still boils down to whether a person eats too much or exercises enough. The danger in bending too far in the direction of a biological explanation — whether that explanation is genetics, infectobesity or some theory yet to be discovered — is that it could be misinterpreted, by fat and thin alike, as saying that behavior is irrelevant.
Jeffrey Gordon, whose theory is that obesity is related to intestinal microorganisms, has never had a weight problem. He’s a rangy man, and when I met him he was dressed in a plaid shirt and clean chinos stretching over long, long legs. He wanted to be an astronaut as a kid, but he was too tall, 6-foot-2 by the time he was a teenager, and he says that back then, NASA was training only astronauts short enough to squeeze into the little space capsules of the day. Gordon has a big friendly face and curly brown hair that make him look younger than 58. He was a competitive swimmer as a child, from age 9 through his undergraduate years at Oberlin, but these days he seems more nerd than athlete: he continually makes puns, for one thing, and he alludes frequently to “Star Trek.”
“Are you ready to begin our Vulcan mind meld?” he asked when he collected me at my hotel in St. Louis, where I went to meet him and his colleagues at the Center for Genome Sciences at Washington University, which he directs. In a way, I was indeed hoping for a mind meld; I wanted to find out everything Gordon knows about the bugs in our guts, and how those bugs might contribute to human physiology — in particular, how they might make some people fat.
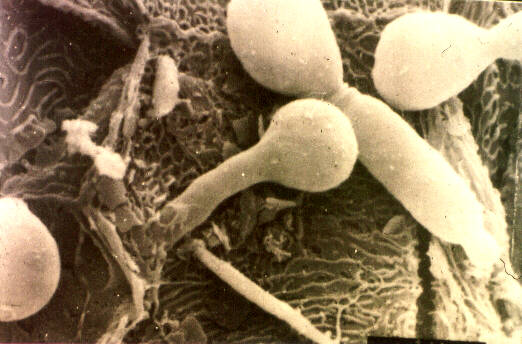
Of the trillions and trillions of cells in a typical human body — at least 10 times as many cells in a single individual as there are stars in the Milky Way — only about 1 in 10 is human. The other 90 percent are microbial. These microbes — a term that encompasses all forms of microscopic organisms, including bacteria, fungi, protozoa and a form of life called archaea — exist everywhere. They are found in the ears, nose, mouth, vagina, anus, as well as every inch of skin, especially the armpits, the groin and between the toes. The vast majority are in the gut, which harbors 10 trillion to 100 trillion of them. “Microbes colonize our body surfaces from the moment of our birth,” Gordon said. “They are with us throughout our lives, and at the moment of our death they consume us.”
Known collectively as the gut microflora (or microbiota, a term Gordon prefers because it derives from the Greek word bios, for “life”), these microbes have a Star Trek analogue, he says: the Borg Collective, a community of cybernetically enhanced humanoids with functions so intertwined that they operate as a single intelligence, sort of like an ant colony. In its Borglike way, the microflora assumes an extraordinary array of functions on our behalf — functions that we couldn’t manage on our own. It helps create the capillaries that line and nourish the intestines. It produces vitamins, in particular thiamine, pyroxidine and vitamin K. It provides the enzymes necessary to metabolize cholesterol and bile acid. It digests complex plant polysaccharides, the fiber found in grains, fruits and vegetables that would otherwise be indigestible.
And it helps extract calories from the food we eat and helps store those calories in fat cells for later use — which gives them, in effect, a role in determining whether our diets will make us fat or thin.
In the womb, humans are free of microbes. Colonization begins during the journey down the birth canal, which is riddled with bacteria, some of which make their way onto the newborn’s skin. From that moment on, every mother’s kiss, every swaddling blanket, carries on it more microbes, which are introduced into the baby’s system.
By about the age of 2, most of a person’s microbial community is established, and it looks much like any other person’s microbial community. But in the same way that it takes only a small percentage of our genome to make each of us unique, modest differences in our microflora may make a big difference from one person to another. It’s not clear what accounts for individual variations. Some guts may be innately more hospitable to certain microbes, either because of genetics or because of the mix of microbes already there. Most of the colonization probably happens in the first few years, which explains why the microflora fingerprints of adult twins, who shared an intimate environment (and a mother) in childhood, more closely resemble each other than they do those of their spouses, with whom they became intimate later in life.
No one yet knows whether an individual’s microflora community tends to remain stable for a lifetime, but it is known that certain environmental changes, like taking antibiotics, can alter it at least temporarily. Stop the antibiotics, and the microflora seems to bounce back — but it might not bounce back to exactly what it was before the antibiotics.
In 2004, a group of microbiologists at Stanford University led by David Relman conducted the first census of the gut microflora. It took them a year to do an analysis of just three healthy subjects, by which time they had counted 395 species of bacteria. They stopped counting before the census was complete; Relman has said the real count might be anywhere from 500 species to a few thousand.
About a year ago, Relman joined with other scientists, including Jeffrey Gordon, to begin to sequence all the genes of the human gut microflora. In early June, they published their results in Science: some 78 million base pairs in all. But even this huge number barely scratches the surface; the total number of base pairs in the gut microflora might be 100 times that. Because there are so many trillions of microbes in the gut, the vast majority of the genes that a person carries around are more microbial than human. “Humans are superorganisms,” the scientists wrote, “whose metabolism represents an amalgamation of microbial and human attributes.” They call this amalgamation — human genes plus microbial genes — the metagenome.
Gordon first began studying the connection between the microflora and obesity when he saw what happened to mice without any microbes at all. These germ-free mice, reared in sterile isolators in Gordon’s lab, had 60 percent less fat than ordinary mice. Although they ate voraciously, usually about 30 percent more food than the others, they stayed lean. Without gut microbes, they were unable to extract calories from some of the types of food they ate, which passed through their bodies without being either used or converted to fat.
When Gordon’s postdoctoral researcher Fredrik Bäckhed transplanted gut microbes from normal mice into the germ-free mice, the germ-free mice started metabolizing their food better, extracting calories efficiently and laying down fat to store for later use. Within two weeks, they were just as fat as ordinary mice. Bäckhed and Gordon found at least one mechanism that helps explain this observation. As they reported in the Proceedings of the National Academy of Sciences in 2004, some common gut bacteria, including B. theta, suppress the protein FIAF, which ordinarily prevents the body from storing fat. By suppressing FIAF, B. theta allows fat deposition to increase. A different gut microbe, M. smithii, was later found to interact with B. theta in a way that extracts additional calories from polysaccharides in the diet, further increasing the amount of fat available to be deposited after the mouse eats a meal. Mice whose guts were colonized with both B. theta and M. smithii — as usually happens in humans in the real world — were found to have about 13 percent more body fat than mice colonized by just one or the other.
Gordon likes to explain his hypothesis of what gut microbes do by talking about Cheerios. The cereal box says that a one-cup serving contains 110 calories. But it may be that not everyone will extract 110 calories from a cup of Cheerios. Some may extract more, some less, depending on the particular combination of microbes in their guts. “A diet has a certain amount of absolute energy,” he said. “But the amount that can be extracted from that diet may vary between individuals — not in a huge way, but if the energy balance is affected by just a few calories a day, over time that can make a big difference in body weight.”
In another line of research, Gordon and his postdoctoral researcher Ruth Ley compared the microflora in two kinds of mice: normal-weight mice and mice with a genetic mutation that made them fat. Like humans, the mice had microflora consisting almost exclusively of two divisions of bacteria, the Bacteroidetes and the Firmicutes. But the proportions differed depending on whether the host was thin or fat. The normal-weight mice had more Bacteroidetes than Firmicutes in their gut microflora. The genetically obese mice had the opposite proportions: 50 percent fewer Bacteroidetes, 50 percent more Firmicutes.
It isn’t clear what the functional significance is of having more Firmicutes in the gut, nor whether the observed difference is a cause of the obesity or an effect. But Gordon wanted to see whether something comparable happened in humans of different weights. Over the past year, he and his colleagues have evaluated stool samples from 12 obese patients at a weight-loss clinic at Washington University, along with some normal-weight controls. They want to see if there’s such a thing as lean-type and obese-type microflora, and whether weight loss leads to a change in a person’s microbial community.
Gordon says he is still far from understanding the relationship between gut microflora and weight gain. “I wish you were writing this article a year from now, even two years from now,” he told me. “We’re just beginning to explore this wilderness, finding out who’s there, how does that population change, which are the key players.” He says it will be a while before anyone figures out what the gut microbes do, how they interact with one another and how, or even whether, they play a role in obesity. And it will be even longer before anyone learns how to change the microflora in a deliberate way.
You might think a microbial theory of obesity could change people’s views about the obese, perhaps even lessen the degree to which people think that obesity is the fat person’s own fault. But anti-fat sentiments seem to be deeply ingrained and resistant to change, as reflected in a rather unlikely place: New Scientist, a British magazine. In an article last year describing the work of Gordon and two groups of researchers in England who were also investigating the link between obesity and gut microflora, the author, Bijal Trivedi, was quite sympathetic to Gordon’s hypothesis. But the article — which is, remember, about a possible biological cause of obesity — was presented with a headline that still managed to depict obese people as lazy and gluttonous. It was called “Slimming for Slackers” and was illustrated with a fat man in a sweatsuit — the “slacker” of the title — sitting beside a partly eaten chocolate doughnut, waiting passively for thinness to arrive.
This is not to single out the New Scientist editors; they are just reflecting the generalized belief that there’s an element of laziness in anyone’s obesity. “Gluttony and sloth are two of the seven deadly sins,” said Ellen Ruppel Shell, author of “The Hungry Gene.” “We ascribe obesity to a character flaw.” This is what leads to the psychic pain of being fat, the social isolation of having a condition that everyone believes to be completely within your control — as if it were a voluntary purgatory, a case of willfully digging your own grave with your dinner fork.
I found that this attitude exists even among obese people, including a woman who was a research subject in Gordon’s clinical study. Joan was one of the obese patients at Washington University who sent Gordon stool samples as she lost weight (15 pounds over the course of a year, which she eventually gained back when she stopped dieting) so they could be tested for various microbes. She said she hasn’t been curious enough to try to find out about her microflora; she’s too busy, and besides, she already knows where to place the blame for her excess weight — not on a microbe but on herself. “I know that I’m not being obedient, I’m not using my body the way God intended,” said Joan, who asked me to refer to her only by her middle name. “I know how I’m supposed to eat, but I’m not having a healthy appetite, you know what I’m saying? I’m not wanting to be obedient.”
But it’s not about obedience — or at least not only about obedience. “The biochemistry of the body of the obese person is very different from that of a lean person,” said Richard Atkinson, Janet S.’s former physician. “If the obese person gets down to a lean person’s weight, their biochemistry is not the same.” Losing weight is hard, keeping it off is harder and, especially for some unfortunate souls, the body seems to work against itself in the struggle.
There’s another way that biological middlemen might be involved in obesity — in this case, not the gut microbes (mostly bacteria) with which we co-exist but the viruses and other pathogens that occasionally infect us and make us ill. This is the subspecialty that is being called infectobesity.
The idea of infectobesity dates to 1988, when Nikhil Dhurandhar was a young physician studying for his doctorate in biochemistry at the University of Bombay. He was having tea with his father, also a physician and the head of an obesity clinic, and an old family friend, S. M. Ajinkya, a pathologist at Bombay Veterinary College. Ajinkya was describing a plague that was killing thousands of chickens throughout India, caused by a new poultry virus that he had discovered and named with his own and a colleague’s initials, SMAM-1. On autopsy, the vet said, chickens infected with SMAM-1 revealed pale and enlarged livers and kidneys, an atrophied thymus and excess fat in the abdomen.
The finding of abdominal fat intrigued Dhurandhar. “If a chicken died of infection, having wasted away, it should be less fat, not more,” he remembered thinking at the time. He asked permission to conduct a small experiment at the vet school.
Working with about 20 chickens, Dhurandhar, then 28, infected half of them with SMAM-1. He fed them all the same amount of food, but only the infected chickens became obese. Strangely, despite their excess fat, the infected obese chickens had low levels of cholesterol and triglycerides in their blood — just the opposite of what was thought to happen in humans, whose cholesterol and triglyceride levels generally increase as their weight increases. After his pilot study in 1988, Dhurandhar conducted a larger one with 100 chickens. It confirmed his finding that SMAM-1 caused obesity in chickens.
But what about humans? With a built-in patient population from his clinic, Dhurandhar collected blood samples from 52 overweight patients. Ten of them, nearly 20 percent, showed antibody evidence of prior exposure to the SMAM-1 virus, which was a chicken virus not previously thought to have infected humans. Moreover, the once-infected patients weighed an average of 33 pounds more than those who were never infected and, most surprisingly, had lower cholesterol and triglyceride levels — the same paradoxical finding as in the chickens.
The findings violated three pieces of conventional wisdom, Dhurandhar said recently: “The first is that viruses don’t cause obesity. The second is that obesity leads to high cholesterol and triglycerides. The third is that avian viruses don’t infect humans.”
Dhurandhar, now 46, is a thoughtful man with a head of still-dark hair. Like Gordon, he has never been fat. But even though he is so firmly in the biological camp of obesity researchers, he ascribes his own weight control to behavior, not microbes; he says he is slim because he walks five miles a day, lifts weights and is careful about what he eats. Being overweight runs in his family; Dhurandhar’s father, who still practices medicine in India, began treating obese patients because of his own struggle to keep his weight down, from a onetime high of 220.
Slim as he is, Dhurandhar nonetheless is sensitive to the pain of being fat and the maddening frustration of trying to do anything about it. He takes to heart the anguished letters and e-mail he receives each time his research is publicized. Once, he said, he heard from a woman whose 10-year-old grandson weighed 184 pounds. The boy rode his bicycle until his feet bled, hoping to lose weight; he was so embarrassed by his body that he kept his T-shirt on when he went swimming. The grandmother told Dhurandhar that the virus research sounded like the answer to her prayers. But the scientist knew that even if a virus was to blame for this boy’s obesity, he was a long way from offering any real help.
In 1992, Dhurandhar moved his wife and 7-year-old son to the United States in search of a lab where he could continue his research. At first, because infectobesity was so far out of the mainstream, all he could find was unrelated work at North Dakota State University. “My wife and I gave ourselves two years,” he recalled. “If I didn’t find work in the field of viruses and obesity in two years, we would go back to Bombay.”
Dhurandhar’s battle against the conventional wisdom was reminiscent of the struggle a decade earlier of two Australian scientists, who were also proposing an infectious cause for a chronic disease, in their case, a bacterium that causes ulcers. The Australians were met with skepticism at first, but eventually they accumulated enough evidence to make it hard to ignore the connection between ulcers and the bacterium, Helicobacter pylori. It helped that one of them, Barry J. Marshall, dramatically swallowed a pure culture of H. pylori — and promptly came down with symptoms of gastritis, the first stage of an ulcer. (The H. pylori story ended with the ultimate vindication: Marshall and his collaborator, J. Robin Warren, won the Nobel Prize in 2005.)
One month before his self-imposed deadline in 1994, Dhurandhar received a job offer from Richard Atkinson, who was then at the University of Wisconsin, Madison. Atkinson, always on the lookout for new biological explanations of obesity, wanted to collaborate with Dhurandhar on SMAM-1. But the virus existed only in India, and the U.S. government would not allow it to be imported. So the scientists decided to work with a closely related virus, a human adenovirus. They opened the catalogue of a laboratory-supply company to see which one of the 50 human adenoviruses they should order.
“I’d like to say we chose the virus out of some wisdom, out of some belief that it was similar in important ways to SMAM-1,” Dhurandhar said. But really, he admitted, it was dumb luck that the adenovirus they started with, Ad-36, turned out to be so fattening.
By this time, several pathogens had already been shown to cause obesity in laboratory animals. With Ad-36, Dhurandhar and Atkinson began by squirting the virus up the nostrils of a series of lab animals — chickens, rats, marmosets — and in every species the infected animals got fat.
“The marmosets were most dramatic,” Atkinson recalled. By seven months after infection, he said, 100 percent of them became obese. Subsequently, Atkinson’s group and another in England conducted similar research using other strains of human adenovirus. The British group found that one strain, Ad-5, caused obesity in mice; the Wisconsin group found the same thing with Ad-37 and chickens. Two other strains, Ad-2 and Ad-31, failed to cause obesity.
In 2004, Atkinson and Dhurandhar were ready to move to humans. All of the 50 strains of human adenoviruses cause infections that are usually mild and transient, the kind that people pass off as a cold, a stomach bug or pink eye. The symptoms are so minor that people who have been infected often don’t remember ever having been sick. Even with such an innocuous virus, it would be unethical, of course, for a scientist to infect a human deliberately just to see if the person gets fat. Human studies are, therefore, always retrospective, a hunt for antibodies that would signal the presence of an infectious agent at some point in the past. To carry out this research, Atkinson developed — and patented — a screening test to look for the presence of Ad-36 antibodies in the blood.
The scientists found 502 volunteers from Wisconsin, Florida and New York willing to be screened for antibodies, 360 of them obese and 142 of them of not obese. Of the leaner subjects, 11 percent had antibodies to Ad-36, indicating an infection at some point in the past. (Ad-36 was identified relatively recently, in 1978.) Among the obese subjects, 30 percent had antibodies— a difference large enough to suggest it was not just chance. In addition, subjects who were antibody-positive weighed significantly more than subjects who were uninfected. Those who were antibody-positive also had cholesterol and triglyceride readings that were significantly lower than people who were antibody-negative — just as in the infected chickens — a finding that held true whether or not they were obese.
Were fat people just more prone to infection? Probably not, because the scientists also screened for antibodies to two other strains of adenovirus, and there was no difference between those who were obese and those who were not. Could the differences be explained by genes instead of by viruses? Probably not, because the scientists controlled for genes in a follow-up study that involved 90 pairs of twins. In the twin study, they found 20 identical-twin pairs who were “discordant” for antibodies to Ad-36, meaning one twin had been exposed to the virus and the other twin had not. In the discordant pairs, the infected twin tended to be fatter, with an average of almost 2 percent more body fat (29.6 percent versus 27.5 percent) than the uninfected twin — even though they shared exactly the same genes.
If Ad-36 is a cause of obesity, Atkinson says, you’re more likely to catch it from a newly infected and still-contagious thin person than from someone who has already gained weight because of its effects. Exactly what the virus does to create this kind of long-term perturbation is still being investigated. In a paper published last year in The International Journal of Obesity, Atkinson and Dhurandhar, along with five of their colleagues, presented evidence for how Ad-36 might affect fat cells directly, “leading to an increased fat-cell number and increased fat-cell size.”
As for the other pathogens implicated in infectobesity — nine in all — certain viruses are known to impair the brain’s appetite-control mechanism in the hypothalamus, as happens in some cases of people becoming grossly obese after meningitis. Scientists also point to a commonality between fat cells and immune-system cells, although the exact significance of the connection is unclear. Immature fat cells, for instance, have been shown to behave like macrophages, the immune cells that engulf and destroy invading pathogens. Mature fat cells secrete hormones that stimulate the production of macrophages as well as another kind of immune-system cell, T-lymphocytes.
Another line of investigation in the field of infectobesity concerns inflammation, a corollary of infection. Obese people have higher levels of two proteins related to inflammation, C-reactive protein and interleukin-6. This may suggest that an infectious agent has set off some sort of derangement in the body’s system of fat regulation, making the infected person fat. A different interpretation is not about obesity causation but about its associated risks. Some scientists, including Jeffrey Gordon’s colleagues at Washington University, are trying to see whether the ailments of obesity (especially diabetes and high blood pressure) might be caused not by the added weight per se, but by the associated inflammation.
Infectobesity has its critics, among them Stephen Bloom, a researcher at Imperial College London. Bloom said that if he were working at a research agency, he’d give money for studies into the viral causes of obesity, just in case there’s something there. But he said he wouldn’t put the theory into a medical-school textbook just yet. His main objection, he said, is that “I don’t think we need that explanation, since we have a perfectly good other explanation.” Like Dhurandhar and Atkinson, Bloom suspects that obesity has a biological cause — but rather than turning to gut microflora or adenovirus infection for an explanation, he is partial to what he calls “the lazy-greedy gene” hypothesis, his slightly disparaging shorthand for what is more generally known as the thrifty genotype.
The thrifty-genotype hypothesis holds that there was, once upon a time, an adaptive advantage to being able to get fat. Our ancestors survived unpredictable cycles of food catastrophes by laying down fat stores when food was plentiful, and using up the stores slowly when food was scarce. The ones who did this best were the ones most likely to survive and to pass on the thrifty genotype to the next generation. But this mechanism evolved to get through a difficult winter — and we’re living now in an eternal spring. With food so readily available, thriftiness is a liability, and the ability to slow down metabolism during periods of reduced eating (a k a dieting) tends to create a fatter populace, albeit a more famine-proof one.
Bloom, by the way, does not give much credence to Dhurandhar’s analogy between the Ad-36-obesity connection and the recent history of H. pylori and ulcers — even though each started out looking like just another wacky idea. “There are so many crazy theories,” he said. “But just because one in a hundred turns out to be correct doesn’t mean all the crazy theories are correct.”
Obesity has turned out to be a daunting foe. Many of us are tethered to bodies that sabotage us in our struggle to keep from getting fat, or to slim down when we do. Microbes might be one explanation. There might be others, as outlined in June in a paper in The International Journal of Obesity listing 10 “putative contributors” to obesity, among them sleep deprivation, the increased use of psychoactive prescription drugs and the spread of air-conditioning.
But where does this leave us, exactly? Whatever the reason for any one individual’s tendency to gain weight, the only way to lose the weight is to eat less and exercise more. Behavioral interventions are all we’ve got right now. Even the supposedly biological approach to weight loss — that is, diet drugs — still works (or, more often, fails to work) by affecting eating behavior, through chemicals instead of through willpower. If it turns out that microbes are implicated in obesity, this biological approach will become more direct, in the form of an antiviral agent or a microbial supplement. But the truth is, this isn’t going to happen any time soon.
On an individual level and for the foreseeable future, if you want to lose weight, you still have to fiddle with the energy equation. Weight still boils down to the balance between how much a particular body needs to maintain a certain weight and how much it is fed. What complicates things is that in some people, for reasons still not fully understood, what their bodies need is set unfairly low. It could be genes; it could be microbes; it could be something else entirely.
Janet S. is one such person. Thirty years after her obesity surgery, 170 pounds lighter than when she started, she still needs to restrict her food intake to keep from gaining it all back.
“I definitely have to diet — damn it, I should have a pass on that, don’t you think?” said Janet, now 55, a human-resources administrator in Southern California, married and with a teenage daughter who is tall and slender. Even with the surgery, and even maintaining a weight that is borderline obese (at least according to the government definition; Janet weighs 180 pounds, plus or minus 15, meaning her body-mass index hovers around the magic number of 30), she can never enjoy food with complete and carefree abandon.
This is typical of people who have lost weight — not only a lot of weight, as Janet has, but even a little weight. According to Rudolph Leibel, an obesity researcher at Columbia University who was involved in the discovery of the first human gene implicated in obesity, if you take two nonobese people of the same weight, they will require different amounts of food depending on whether or not they were once obese. It goes in precisely the maddening direction you might expect: formerly fat people need to eat less than never-fat people to maintain exactly the same weight. In other words, a 150-pound woman who has always weighed 150 might be able to get away with eating, say, 2,500 calories a day, but a 150-pound woman who once weighed more — 20 pounds more, 200 pounds more, the exact amount doesn’t matter — would have to consume about 15 percent fewer calories to keep from regaining the weight. The change occurs as soon as the person starts reducing, Leibel said, and it “is not proportional to amount of weight lost, and persists over time.”
For many people, then, losing weight and keeping the weight off requires a constant state of hunger — and when you’re hungry, you’re miserable. You think of nothing but food every moment of the day. All morning you think about lunch, all afternoon you think about dinner, and when you’re asleep, you dream of food.
Or, as Judith Moore put it in her memoir, “Fat Girl”: “Some people daydream heroic deeds or sex scenes or tropical vacations. I daydream crab legs dipped in hot butter.” She wrote about fellow warriors who, like her, struggle to keep off the weight they worked so hard to lose. As they approach the all-you-can-eat buffet, she wrote, “they square their shoulders. They ready for combat with Virginia baked ham, sweet-potato soufflé and those puffy dinner rolls with butter and a three-layer chocolate mousse cake. Food is the enemy. Food is also the mother, the father, the warmhearted lover, the house built of redbrick that not even the wolf can blow down.”
Current public-health messages deny this harsh reality. They make losing weight sound easy, just a simple matter of doing the math and applying some willpower. A pound of fat contains 3,500 calories, government documents say, and if you cut down a week’s worth of food intake or increase exercise by a total of 3,500 calories, then, voilà — you lose a pound. “To lose weight, you must use more energy than you take in,” states the Web site of the Office of the Surgeon General. “A difference of one 12-oz. soda (150 calories) or 30 minutes of brisk walking most days can add or subtract approximately 10 pounds to your weight each year.”
But if genes or viral infection or gut microflora are involved, then for some people 3,500 calories might not equal a pound of fat, and 150 fewer calories a day might not mean they’ll lose 10 pounds in a year. As scientists continue to investigate how obese people are different, we can only hope that a side benefit will be a more largehearted understanding of what it means to be fat and how hard it is to try to become, and to remain, less fat.
A more concrete benefit would be to develop ways to interfere with the action of the offending microbes. Atkinson, for one, foresees a day when Ad-36 antibody screening becomes as routine as cholesterol screening. He has a financial stake in making this happen; when he moved to Virginia two years ago, he started a company called Obetech to market his Ad-36 antibody test, for which he charges $450. But he said he has an altruistic motive as well. The people most likely to benefit from such testing, he said, are not fat people but thin people, whose infections are so recent that they haven’t yet begun to gain weight. But they are the least likely to pay to have it done without it being part of a routine checkup.
Based on animal studies, Atkinson assumes that people infected with Ad-36 have a better than even chance of becoming obese. “But if they watch their diet, and if they exercise, they can avoid it.” Further in the future, he said, there might be a way to administer antiviral drugs to infected individuals early enough to block the effect of Ad-36 on the fat cells.
Gordon, too, is hoping that his research will eventually lead to new strategies for treating obesity. It’s a long way off, he said, but it’s the beacon that keeps him and his colleagues working.
“How can you manipulate the microbial community to more broadly affect energy balance?” he asked, enumerating the research questions still to be tackled. “Can one size fit all, or can you match nutrition to the microbes in your gut?” After obese-type microflora are differentiated from lean-type, Gordon said, the next step would be what he calls “personalized nutrition” — matching diet to the digestive properties of each person’s unique microflora.
Such deliberate manipulation of the gut microflora is a long way off — years and years off, according to Gordon — but its possibility “is what this first phase of our work is underscoring, and we hope it will turn out to be an important tool in the fight against obesity.”
Link: http://www.nytimes.com/2006/08/13/magazine/13obesity.html?_r=1&oref=slogin