Cavitations & Root Canals – Interview With Dr. Meinig and Dr. LaMarche
Another great article with Dr Meinig and Dr. LaMarche where you can find out more about danger of root canals in our teeth, cavitations that stay after dentists remove the tooth and the danger of cavitations. Also you can read more about Dr. Price who was the first one to prove the dangers or root canals and cavitations in our mouth. After reading this material I am sure I will not allow any root canal to be done in my mouth. I rather have the tooth extracted. After the cavitations were cleaned and root canals removed the infections in the body disappeared. Also many health problems vanished. I published this article in two parts because of its length. Read the article …….
Laura Lee: Have you ever looked at fossil remains of dinosaurs or those of early man and noticed those rows and rows of perfect teeth still intact? Have you ever wondered why modern man can’t seem to get through a lifetime with all his teeth intact, it doesn’t seem fair does it? What are we doing wrong?
No doubt you’ve heard and we have covered in depth on this show the problems arising from mercury and silver amalgams. It’s so well known in fact that 50% of the over 1,000,000 amalgams placed in teeth of Americans today are composites. A new material that doesn’t contain mercury.
You probably thought that mercury was the big issue and that now you know about it you’re safe in terms of what’s safe in your mouth. I’m sorry, but there’s more. There’s much, much more. And we have tonight two gentlemen who are experts in their field in some of the newest research, actually it’s old research, but it’s just getting the attention today that it deserves.
And that is problems with root canals; apparently there are bacteria that can be harbored in root canals no matter how perfectly they’re done. These bacteria mutate and become toxin factories, they can get out into the bloodstream and cause degenerative diseases or make them worse.
Also cavitation is a new term you’re going to learn tonight and that is the space left in the jawbone when a tooth is extracted. If an infected tooth or simply a wisdom tooth that needs to come out to make space, problems can arise with dead tissue in the jawbone and you’re going to learn tonight what you can do about these conditions. We have with us Dr. George Meinig, the author of Root Canal Cover-Up. It’s a book that details this work from the 1920’s done by Dr. Westin Price. Research that has been done recently and confirmed. He’s a specialist in root canals and a dentist.
We also have with us Dr. Michael LaMarche. He’s a dentist that is in practice today specializing in mercury removal. He has worked closely with Dr. Hal Huggins who’s a leading researcher into mercury toxicity and silver dental amalgams and also Dr. LaMarche is one of 13 dentists selected nationwide selected for research into cavitations. And we’re going to find out some very important and useful information tonight.
Welcome Dr. Meinig.
Dr. Meinig: Thank you very much, Laura.
Laura Lee: And welcome Dr. LaMarche.
Dr. LaMarche: Thank you, it’s a pleasure to be here.
Laura Lee: Thank you for all the work that you two have been doing in this. I know that people who are plagued with degenerative diseases, people who want to avoid those conditions, people whose health is delicate don’t need any extra assaults on the immune system.
And this research is quite startling when you first hear about it. It begins to make more and more sense when you look into it. Let’s start with you Dr. Meinig, tell us a bit about the problems with root canals, your research and why do we even have infected teeth? That’s a question we’ll get to – prevention – at the end of our discussion tonight, but what is a root canal, let’s define some terms. What has been some of the research?
Dr. Meinig: Let me start out by saying that I am one of the 19 founding members of the root canal association, so the people out there don’t get the idea that I have no background in the…
Laura Lee: Did I not mention that? I’m sorry, that was in my notes.
Dr. Meinig: And it’s important for you to know that because I’m going to be saying some things critical about root canal treatment today. And the reason is that I practiced some 47 years and in all of that time I never heard about a 25-year research program that was conducted by Dr. Westin Price in the early 1900’s and actually before then and it was finally published in 1923.
His work was all well documented in two volumes of 1174 pages and in 25 articles that appear in the medical and dental literature. Now what he reported and what he found with the tests which involved some 5,000 animals over the 25 year period was root canal distilled teeth, no matter how good they looked, or how free they were from symptoms, always remained infected.
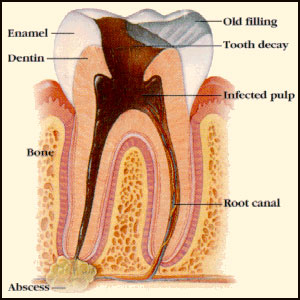
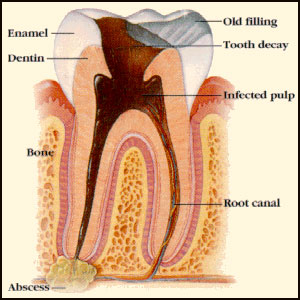
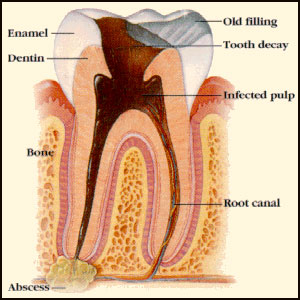
Now that’s a shocker, and it’s one that many dentists don’t want to believe because many of the things that we do as an endodontist involve large areas of bone loss at the end of a root of the tooth and when you do the root canal filling you see that bone fills in with new bone and how could that dentist and that patient ever think that there could still be infection in that tooth? And the problem is that the infection occurs in what is known as the dentin of the tooth.
The dentin involves 95% of all of the tooth substance and surprisingly, although it’s almost as hard as enamel when it’s cut with a drill it makes a shrill noise just like if you were cutting stone, and you would think it was a very hard solid substance. Surprisingly it’s composed of little tiny tubules, and those tubules are so small that if we took our smallest front tooth and stretched it out – stretched those tubules out end to end – it would stretch out for a distance of 3 miles.
Now what happens is when you get a cavity in a tooth and the decay gets into the dentin of the tooth the bacteria that are involved in the decay process get into those tubules. I should tell you that initially those tubules carry a fluid and that that fluid carries nutriments and the nutriments in those dentin tubules keep the tooth alive and healthy.
And those nutriments come from the nerve and the blood vessels that come into the root canal of the tooth. And so fundamentally what happens when you get a deep cavity and it exposes the nerve of the tooth, those bacteria get into all of those dentin tubules and they remain in there causing infection and eventually they can escape and that’s a story in itself. They can escape in what’s known as the lateral canals and there toxins can actually escape directly through the root surface into what’s called the peridontal membrane or ligament.
This is a hard fibrous tissue which holds the tooth in the bony socket, and when the infection gets into there it transfers easily into the bony socket and from there the bacteria and the bacterial toxins can get into the surrounding bone and the blood supply of that surrounding bone. And now this acts much like cancer cells, you know cancer cells metastasize and that means that they travel around the body in the bloodstream and they get to another tissue, gland or organ and they set up a new cancer.
Well these bacteria from infected dentin tubules also travel around and metastasize in the same way and they can get into the various tissue. Those bacteria are kind of like people, you know, if they get to like Seattle or Reno or someplace they decide that’s where they’re going to have their home, well the bacteria traveling around the body, they may get to the liver, the kidneys or the heart or the eyes or some other tissue and they set up an infection in that area. So this is exactly what happens and why the degenerative diseases occur from these teeth.
Laura Lee: Now why isn’t the immune system not able to knock out these bacteria when they get outside the tooth? I can understand three miles of tunnels in these microtubules of an infected tooth for these bacteria to propagate in. It’s hard for the immune system to get in there, but once they travel out, what’s the immune system doing there? Just a slow wear and tear where they can’t get rid of the infection sites so it’s this constant default…?
Dr. Meinig: Well, you’re right, the immune system under certain circumstances can take care of this quite adequately, but it has to be those people who have extremely good genetic backgrounds who are in good nutrition basis, are having no health problems, in their daily life.
Laura Lee: Now, who in the late 20th century can make that claim with all the assaults on our systems.
Dr. Meinig: That’s right, Laura, there’s not very many that can make that claim. Now if there are some people, and Dr. Price found that 258 of his patients met that requirement, he found they could stand root canals for many years without any difficulty until they had a severe accident, until they got a case of the flu, they had some severe stress to them, and now their immune system which was able to cope with these bacteria and these toxins of the bacteria now had too much to do and they could no longer cope and this person would develop a disease in their liver, their kidneys, their eyes, their brain, their whatever, just the same as a cancer metastasizing around this would happen to them in degenerative disease situation.
And yet it’s counter intuitive to what dentists observe, or how we thought the mouth worked, or bacteria in the immune system worked. So I’d like to know what’s the original research, I know he did a lot with rabbits, it’s pretty startling research, it’s dramatic research. Let’s talk about that and how it went on for so long and you said there was a cover-up involved. We’ve got more to talk about with Dr. George Meinig, the author of Root Canal Cover-up and Dr. Michael LaMarche that’s going to tell us a bit about cavitations. I’m Laura Lee.
Michael, you were telling me in the break that your description of your practice in dentistry is now encompassing so much more that you now describe it as biologically compatible dentistry. Could you define that term and then we’ll…
Dr. LaMarche: Yes, basically our practice has changed and to say that our focus was strictly on amalgam removal would not be correct. I think we’re more focused on the nutritional aspects of an individual in conjunction with blood chemistries and also working very closely with physicians for the patient’s general overall health. Certainly we are concerned with heavy metals in our patients but to say that would be our major concern and focus would…
Laura Lee: Well, I’m one of your patients and I know that you look at the system as a holistic system and that the role that dental health plays in that segues into so many other areas so I think you’re the dentist of the future and that you’re looking at the whole system of the person, the entire health of the person, and that interplays, yes indeed. Thank you for making that correction. And you’ll also find Dr. LaMarche in Lake Stevens, Washington. Dr. Meinig, you were going to tell us about Westin Price’s work in the 1920’s – how he even happened onto the thought that root canals might be a stress on the immune system.
Dr. Meinig: Before I mention that I should say that all of this is really dealing with the theory of local infection. Focal infection means that you can have an infection somewhere in the body and that the bacteria that are involved may be transferred to another tissue, gland, or organ somewhere in the body and set up a whole new infection. Most of this was started by Dr. Billings in the first decade of this century and by 1914 his research had showed that 958 of all focal infections came from teeth and from tonsils.
The others came from a few other sources like infected sinuses, fingernails, toenails, appendices and so on. But what happened is that of course Dr. Price learned about all of this work and he had done a root canal filling for a woman who developed a severe arthritic condition. She was so bad that she was bedridden most of the time and her hands were so swollen with arthritis that she could hardly feed herself. And when he heard about all of this focal infection work by Billings he realized that maybe this root fill that he did that looked so fine on the X-rays was part of her problem in causing this arthritis. And so like all research programs in which researchers get involved, there’s usually one that sets of the tone and this case happened to be the one that captured everybody’s imagination.
There were a lot of others, but this one did, and the reason was that he finally convinced her that she should have that tooth removed and she came into his office, had the tooth removed aseptically incidentally, because if he contaminates the tooth when he’s taking it out with the saliva and other things then that’s a problem of introducing other bacteria into the situation.
Laura Lee: Also couldn’t do a proper lab test on it.
Dr. Meinig: So he did that and he secured a laboratory animal and in this case it was a rabbit and he put a little local anesthetic under the skin of the back of the rabbit. He made a small buttonhole incision into the skin of the rabbit and he put that extracted root canal filled tooth into that incision. He put a couple of little stitches in there to hold the tooth, to keep it from popping out again and he returned the animal to a spacious cage that had plenty of good food and awaited development.
Well it didn’t take long, two days later that rabbit developed the same arthritis in its limbs that the patient had and in ten days it passed away from the infection from that root filled tooth. Well now this was somewhat of a confirmation for Dr. Price that people who had root canal filled teeth and had illnesses that the medical profession was having difficulty in solving – that maybe these root filled teeth were causing those problems, and so whenever he had people who were going from doctor to doctor and not finding out what was wrong with them, he would then advise them to have any root filled teeth out and he would implant the tooth under the skin of the rabbit or they used numbers of other animals, but rabbits proved to be a little more dramatic, but the same thing happened whether it was a dog or a rat or a chipmunk or whatever they used, these same diseases would occur.
Well the surprising thing was when the patient with a heart condition came in and had a root filled tooth and wasn’t getting anywhere with his treatment and they took that root filled tooth and implanted it under the skin of a rabbit, by golly, that rabbit got a heart condition and usually passed away within a few days.
If the person had kidney trouble, well the rabbit got kidney trouble. And if the person had trouble with their eyes, well the rabbit got trouble with the eyes. As a matter of fact the eyes reacted so severely that even minor problems with the patient’s eyes would cause the rabbit to go blindusually in two to three days. And so there were a lot of different situations and almost any disease that you might think of they eventually transferred from a patient through the root filled tooth into another laboratory animal.
Laura Lee: So what’s the theory with the focal infection? Why is it there’s the connection with the infected tooth and that problem area in another part of the body?
Dr. Meinig: Well, the reason that this is a focal infection is because the infection came from the tooth and traveled from the tooth to the heart or the kidneys or the lungs or some area of the body and it set up a new infection.
Laura Lee: Right, but certain bacteria that is human transferred to an animal, say rabbit, that same bacteria will not just accidentally go attack the liver, it will attack the eyes.
Dr. Meinig: Yes.
Laura Lee: It’s destined for that one organ. How do you explain that?
Dr. Meinig: Price I’m sure was not able to explain that either, it was a big surprise to them to think that almost always the same disease occurred. Sometimes it wasn’t exactly the same, but it was usually the same tissue. But most of the time it was actually the same disease and what he did in order to prove these things in those days – he realized he might insert his own thinking into what was happening and so what he did very often was to repeat experiments because they didn’t know double-blind business, but he did know enough about it, so what he did was he transferred…
Laura Lee: We’ll get the rest of this when we come back with DR, George Meinig and Dr. Michael LaMarche. And you thought it was just mercury in your mouth that was a problem. I’m Laura Lee, we’ll be right back on the Laura Lee Show.
And we are back, hi. Dr. George Meinig and Dr. Michael LaMarche are with us in studio tonight. The topic, root canals and the problem with bacteria that get trapped inside the microtubules of the tooth, of an infected tooth, can migrate throughout the body, they can infect an organ, gland or tissue, they can damage the heart, kidneys, joints, eyes, brain. They can even endanger pregnant women. These infections were first discovered by a 25 year root canal research program carried out by the American Dental Association. Dr. Meinig says this research was secretly covered up. It’s been re-examined and redone recently and here’s the story. Let’s start taking some phone calls from Martin up first from Portland, Oregon. Hi, Martin.
Martin: Hello, Laura Lee. Yeah this is kind of a personal topic for me, about 15 years ago I heard a report from the University of Texas Medical School at Waco. They had a 6ve-year study where they demonstrated that 1,000 milligrams of vitamin C per day would prevent periodontal disease.
Well then shortly thereafter my cat came down with distemper so I cured him over a period of ten days using 500 mg. of vitamin C per day. And about two years after that I was diagnosed by my dentist whom I had been going to for a long time, with pretty serious periodontal disease. And he X-rayed my whole mouth upper and lower, showed me all the pockets and everything I had and he sectioned my teeth of into two upper and three lower and did the scraping on the first section lower, the worst part first.
Well I was so frightened and saw that there was going to be such a tremendous amount of expense to me that I immediately started taking 15,000 mg per day for the next four months. He x-rayed my teeth at the end of the third month and he said “You know something’s happening here, the number of pockets you have and the size of those pockets is rapidly diminishing” 90 he wanted to re-X-ray just to verify this, so he did and it showed that some of the smaller pockets had completely gone away and the larger pockets were reduced by less than half their previous size only three months before.
And he was amazed and he asked me what I had been doing, and I said I had simply been taking 15,000 mg of vitamin C every day – 5,000 with each meal. And other than that I hadn’t changed my diet or done anything else. Does your guest have any experience using vitamin C for therapy?
Laura Lee: Well, they are looking into nutrition and the impact it has on health overall. Dr. Meinig…
Dr. Meinig: Well a third of my practice is actually periodontal disease. You said that I was a specialist in endodontics but I preferred to do all of dentistry and about a third of practice was periodontal disease. I never had any patient do 15,000 mg of vitamin C, I got many of them on vitamin C, but not that much, and your discovery is a very interesting one and I’m going to advise a few people to try that and let’s see what happens with them. I can’t say that I’ve had experience to that extent with anybody.
Laura Lee: I would say that you’d want to get the plaque and everything else scraped off your teeth and give yourself a head start. Don’t do it instead of.
Dr. Meinig: That’s right. Absolutely it’s important that you get all of the deposits removed, otherwise…. Incidentally those infections from periodontal pockets are as serious as root canal filled teeth are, so it’s very important that you know that.
Martin: Well, just recently I had had a relapse where one of my front teeth has been pressed back partly out of the jawbone as far as support is concerned and developed a pretty serious periodontal pocket because I used an infected dental floss, well I hadn’t used a brand new one, I used one I used a couple of days previous and apparently the food had become contaminated and it infected the lower gum, down the root line below the gum.
And I developed a pretty serious pus pocket down there which it took about three days to clean out physically, but then I merely started taking high doses of vitamin C and within about 2 weeks the gums are completely cleared up and developed a more reddish color and the tooth was much firmer in the gum than it had been before. Also, ginkgo can have some of the same effect as far as helping a person of middle age or older to develop much stronger teeth, you know as far as being rooted in the jawbone and help their gums .
Laura Lee: Thanks for that story, we appreciate that Martin. Also, let’s go back to the research that Dr. Westin Price had done you were saying you were going to explain another aspect of it.
PART 2
Root canals are not safe. Dr. Meinig is explaining to us that it is impossible to sterilize root canals and kill all the bacteria. So the root canals stay full of anaerobic bacteria that are very harmful to our body, especially when our immune system is damaged. Then these bacteria and viruses travel around the body and the result can be very serious – heart problems, liver diseases, other infections. Read the second parts of the interview with Dr. Meinig on root canals and cavitations. ………
Dr. Meinig: Well, we were talking about the fact that he didn’t know about double-blind studies and what he did instead. He knew that he could introduce his own thinking into what he was doing and so he repeated a lot of things.
For instance he had a patient who had kidney trouble and had a root filled tooth. He removed that tooth, put it under the skin of a rabbit, the rabbit got kidney trouble and died within a few days. He took the tooth out of that rabbit, surgically of course, and washed it in soap and water, disinfected it with a disinfectant and put it under the skin of another rabbit and that rabbit got kidney trouble and passed away. He then took that tooth out of that rabbit and put it in another rabbit and he repeated that 30 times.
Laura Lee: The same tooth?
Dr. Meinig: That’s right. The same root filled tooth. Now the reason he did that was that he had to prove to himself and to the world that this infection was able to be transferred and the only way he knew it was to do more animals and it wasn’t that he disliked rabbits, in fact he took very good care of his rabbits, but this was one way he could do something about it. Now one of the things that happens with these root filled teeth is that when they are removed it is very often that periodontal membrane that is infected and the surrounding bony socket remains in the jaw and sometimes healing gets rid of that but many times it doesn’t. And what happens then is an infection that occurs in the jawbone and I think we should turn this over to Dr. LaMarche because he’s going to be telling you something about that phase of things.
Laura Lee: And the term cavitation. Dr. LaMarche…
Dr. LaMarche: Well cavitation actually is a cavity within the bone which was formerly occupied by a tooth. I think it’s important that our listeners know that our office is one of 30 in the United States, Canada and Europe that have been selected to participate in a research group called the North American NICO Research Group. NICO is an acronym – Neuralgia Inducing Cavitational Osteonecrosis. Which is another word for dead bone, actually it literally means a cavity within the jaw that is lined with dead bone that causes pain.
Our research group was formed by Dr. Jerry Eboco who is an oral pathologist in West Virginia, and he began researching this extensively in I believe early ’90s. Papers have been written on it since the ’80s, and more recently he’s been pursuing this and he gathered together a group of dentists so that we could make the connection between trigeminal neuralgia, atypical facial pain, chronic migraine headaches and cavitations. And what we have found in addition to this is when cavitations are removed, not only do we find that these trigeminal neuralgia’s or this pain is relieved, but we find that patients also realize other improvements within their systemic health.
Laura Lee: How do you remove a cavitation, what do you mean by that? Remove the dead bone?
Dr. LaMarche: Well, cavitations do not show up extremely well on X-ray, but when they are located and maybe a little bit later we can describe how we locate them, but a cavitation is…an incision is made in the gum tissue over where a tooth was formerly located, a large enough area or flap is laid so that the gum is removed from the bone and we are allowed to penetrate the cortical plate or the bone overlying the cavitation. The dental instrument, in this case a drill, will actually fall through the bone and into this cavity. Before we clean it out, however, we go in with an instrument called a curette and scrape it very thoroughly and we submit this sample to the pathologist.
Laura Lee: What kind of lab results do you often get?
Dr. LaMarche: Well, I would say that probably 98% and even larger than 98% what we find is what’s called ischemic osteonecrosis, it’s bone death due to poor perfusion of oxygen or blood supply to a local area. The cavitations are lined with dead bone, the body’s response to that is to…
Laura Lee: Seal it off!
Dr. LaMarche: Seal it off, it does that with fat, we will find fat in there. Ultimately the fat becomes calcified so we see what’s called calcific fat necrosis. We will sometimes see chronic inflammatory cells, however that is not the hallmark of this disease, as a matter of fact we see few inflammatory cells – many times we’ll see bacteria colonies, toxide filaments, within these specimens. I think another very interesting thing that we have learned from this through our biopsying is that the pathologist will identify what he terms fibrin sludging. That is the fibrin will actually start pooling.
Laura Lee: What is fibrin?
Dr. LaMarche: It is the part of the clotting factor and there is some proteins – C proteins, S proteins…
Laura Lee: From blood that was in there when the tooth was pulled?
Dr. LaMarche: Exactly. What happens is the blood initially comes into the site but because of the body’s inability to break down the clot or because of the body’s ability to make a very tenacious clot – one has either what’s called thrombopheha or hypofibrinolysis. Laura Lee: Whichever it is, it doesn’t sound nice.
Dr. LaMarche: Either one of them, one of them is a very tenacious clot or an inability to break the clot down, consequently nothing gets in, nothing gets out, we have bone death.
Laura Lee: Why does it happen in the jaw bone 98% of the time? If someone breaks their leg bone, that bone heals up nicely in most instances. Why does the body have more trouble with the jaw bone tooth extractions than say other parts of the body?
Dr. LaMarche: That’s a very good question. I believe that when a bone is broken and two pieces are put together that’s a different kind of…
Laura Lee: There’s no space left.
Dr. LaMarche: Exactly, however what has been done in the Jewish Hospital in Cincinatti, a Dr. Glick, MD has made a direct correlation between the head of the femur, people fracturing the head of the femur, that osteonecrosis or bone death is identical to that which we find in the jaws.
Laura Lee: Because that’s a more solid part of the bone, a denser part of the bone? What is it about that site?
Dr. LaMarche: I would say that probably it has more to do with the circulation to the area.
Laura Lee: Okay.
Dr. LaMarche: Again, osteonecrosis as we see it is defined as ischemic osteonecrosis and ischemic implies that it is a lack of perfusion of blood to the site.
Laura Lee: In both cases it’s a lack of oxygen that leads to the mutation of the bacteria, they go from being aerobic to being anaerobic bacteria in root canal instances. And here you find a lack of oxygen to the site so there is a common factor. How often do you find where you take out an infected tooth, say a root canal tooth, either it’s infected and you say I don’t want to put a root canal in, let’s pull it and do other options, or it’s a root canal infected tooth that you pull – probably you’re going to have necrotic tissue arising because it’s so full of bacteria, or that compared to say a wisdom tooth that needs to be pulled for other reasons, it’s not infected or impacted – it just needs to get taken out.
Dr. LaMarche: That’s what we’re now recommending no matter why you have to take a tooth out – even if it isn’t infected, then a protocol needs to be followed and that protocol means that the dentist after he removes the tooth he also removes the periodontal ligament or membrane which is a fibrous tissue that holds the tooth in the socket, that’s what keeps the tooth from failing out.
That becomes infected and it’s still attached very securely to the surrounding bony socket and so what we recommend is that the dentist go in with a slow moving drill and remove that periodontal membrane and about 1 mm of the bony socket in order to prevent these infections from occurring. And strangely enough we find in many areas for instance, wisdom teeth when they’re removed, even though they were healthy teeth – for some reason or another they very often develop a cavitation around them.
Some 400/0 of all wisdom teeth extractions develop cavitations and the thing that should be done and what we’re thinking is better to be done, is to remove that periodontal membrane at the time you remove the tooth and some of the surrounding bone in order to prevent this from happening.
Laura Lee: Well, that’s great when you’re getting a tooth extracted by a dentist that knows this research and knows the procedure, but what about all those people who have wisdom teeth? I mean most of us have had our wisdom teeth extracted and they’ve grown over and the dentist didn’t know and so then you have a situation where you probably have to go in again and clean that out as you were describing. We’ll take a break and take some phone calls when we come back and what we’re going to do is have information only about the topic – cavitations, root canals, nutrition.
Root Canals & Cavitations
These are the topics, and please don’t get too personal and ask for a diagnosis. That’s not what these two doctors are here for, but to give out information on some of this new research. We’ll be right back.
Laura Lee: And we are back, hi, Laura Lee here and we are talking with Dr. Michael LaMarche, dentist in Lake Stevens, Washington area and Dr. George Meinig. He’s the author of Root Canal Cover-up, and you were in Ojai, California. We have some calls for you gentlemen, we have Call calling in next. Hi, Call, thanks for joining us.
Gail:Thank you. A couple years ago I had a root canal done and as soon as it was done it didn’t feel very good and I kept telling them I thought something was wrong and they told me it was a great root canal and there was absolutely nothing wrong with it. And I’ve had a lot of pain in my right ear, and the jaw as a result and I can’t find a dentist that’s willing to take that tooth out. I’ve been to three endodontists and five dentists and no one will pull that tooth, because they look at it and say it’s a great root canal. So my question is – where can I find a dentist in my area that will actually look at this and possibly extract that root canal tooth, it’s a bicuspid.
Dr. LaMarche: Can I ask what area she’s in?
Laura Lee: You’re in Tacoma, Washington, Gail?
Gail: Yeah.
Laura Lee: Michael, you mentioned that there were 30 dentists involved in the cavitation research, what about the root canal research? How many dentists are there out there that are up on this and familiar with the work?
Dr. LaMarche: Well currently, right now, in the research group there are 30 of us, and I’m sure that there will be more.
Laura Lee: Can dentists anywhere say “I want to get involved, I want to find out?” They’re looking for more dentists?
Dr. LaMarche: Yes, if they would contact you perhaps you might connect them up with me and we could make arrangements for them to communicate with Dr. Bocho so that they could learn more about this because certainly we need more involved….
Laura Lee: Is there a list available so that someone could send…I’11 be happy to distribute the information, but if there’s a list then our listeners in San Francisco to Minneapolis could also write in and get a list of dentists.
Dr. LaMarche: Exactly. Dr. Bocho did ask those of us participating in this research if we would have any objections to him giving the names out and I cannot recall that anyone raised their hand and objected, so I’m sure that he would provide you with that list.
Laura Lee: And Dr. Meinig do you have any sort of list of dentists who are up on this?
Dr. Meinig: I have a list of dentists that I refer. This is such a new subject many dentists are in disagreement with it of course, because they haven’t heard or seen the research.
Laura Lee: They may disagree until they see the research…
Dr. Meinig: We do have a scattering of them around the country and the only thing is that when we give you a name, the first thing you ask is whether they follow the root canal extraction protocol. Now that may sound like a lot of things to say, but if you just ask if they follow the extraction protocol and they say “yes,” then fine. If they say “no,” then you keep looking, because what you want is somebody that does follow that protocol.
Dr. LaMarche: I would like to add too to this, if I may, that it’s very important that you have that biopsy. I think to take the tooth out, to say we’ve taken care of your problem, or to remove a cavitation and to say that we’ve taken care of the problem is incorrect without substantiating the clinical diagnosis with a pathologist’s report.
Laura Lee: So what do you find out? If you had any bacteria colonies, then what? Then what do you do?
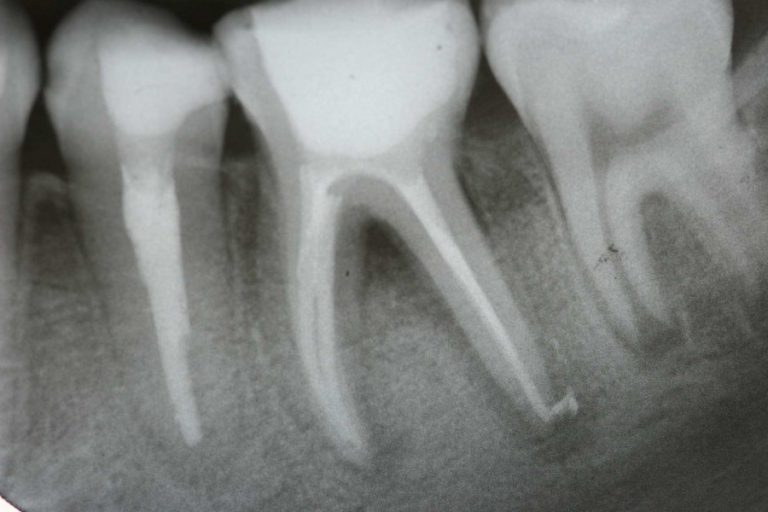
Dr. LaMarche: Well, let me say that for example root canal teeth radiographically on X-ray – they look beautiful, and there are those people that don’t believe that they cause a problem and probably they don’t cause a problem when one is healthy and in a healthy state. I think when root canal teeth become a problem is when one becomes older and there are more immunological challenges. Each root canal tooth that we have removed we have documented on the last 150 – 147 of those have had ischemic osteonecrosis around the tooth.
Dr. Meinig: Is it in the bone around there?
Dr. LaMarche: That is in the bone surrounding the tissue. Laura Lee: Not to mention the tooth itself, right?
Dr. LaMarche: By the way, the trichologist (fungal scientist) also decalcifies the tooth and examines if there is any necrotic or dead tissue within the tooth and some ofthese have been extremely well filled, well done technically.
Laura Lee: Okay, we have Mike calling from a car phone before he gets out of range. Hi, Mike.
Mike: This has been a very interesting topic. My wife is suffering from a probable root canal, but my question is: the research that they did with the animals where they implanted a tooth – how it had affected the kidneys which was the thing of the original patient or whatever – I wanted to know if the original human patient got better or saw improvement after that and after the infected root canal tooth was pulled out.
Dr. Meinig: Sorry I didn’t answer that right away. We get so involved in telling what’s wrong we forget about telling you what happens. Most of these people recover quite quickly, a little of it depends on how long they’ve had the infection. Obviously if they’ve had it for five or ten years it may be pretty well entrenched and take a while to get rid of it and may not get rid of it completely. Most of them however, go away completely and so many of them in one or two days, it’s really very startling.
Some of us are beginning to think that it’s a little more than the transfer of infection and it may be electrical in some way, electrical transference through the acupuncture meridians and through other systems in the body. There are a number of things we don’t know about this, other than we do know that it happens and very many people by the next day – their arthritis is gone. I’ve had them call and tell me that they can now do their mile jogging and walking that they couldn’t do yesterday when they had that tooth in their mouth.
Laura Lee: To me it seems like “hedge your bets.” If there’s this kind of research on line, take advantage of it and this information. Hi, Laura Lee here for a second hour to spend with Dr. George Meinig and Dr. Michael LaMarche talking about cavitations, that space left in the jawbone when a tooth is extracted can lead to having necrotic dead bone tissue there, can lead to jaw pain, neck pain, other problems. And also root canals, the theory being that, in fact this is pretty much confirmed, it’s not really a theory, it’s confirmed science, is it not, Dr. Meinig?
Dr. Meinig: Well, Dr. Price used 5,000 animals to help with all of this confirming.
Laura Lee: And he ran through those rabbits. The research indicating that microtubules in the tooth can harbor bacteria that mutate and that can get out into the bloodstream and cause problems and compromise the immune system and lead to degenerative diseases.
So, we’re going to find out what to do, how to prevent problems and the first place is – nutrition can play a role. I know that you also did some extensive research with Dr. Price’s theory that nutrition impacts the development of the jaw and the person, the personality. An extraordinary amount of research done that is being confirmed today.
By the way, someone wanted to know about getting a list of dentists in your area that is upon this research and can perform some ofthese techniques. There is a list from Dr. Bocho who is heading up the NICO research of which Dr. LaMarche is a member, one of those 30 dentists nationwide who is conducting research into cavitations. And that’s one reason why you’re doing the biopsies and sending it to the lab, because that’s part of the research. You want to know…
Dr. LaMarche: May I add something here – that Dr. Bocho and our group has applied for a grant and we are waiting to hear from NIH, the National Institutes of Health, regarding acceptance of this grant. And it looks as though they’re very excited in supporting us in our research.
Laura Lee: So this is very mainstream then?
Dr. LaMarche: Yes, it is.
Laura Lee: It’s not alternative research when we have the National Institutes of Health involved.
Dr. LaMarche: No. This makes very good sense, what’s happening, and you can’t lie with microscopic slides.
Laura Lee: There are two lists – the Dr. Bocho list of dentists, those 30 dentists in the area, and also the Price-Pottenger list of those who specialize in root canal removal problems.
Dr. LaMarche: Right.
Laura Lee: Okay, we have two lists available and if you send a self-addressed, stamped envelope to me at P.O. Box 3010, Bellevue, Washington 98009 we’ll be happy to send you those two lists. Let’s take a call next from Alex calling from Salt Lake City, KCNR, hi Alex.
This was an interview from the Laura Lee Show on radio that has been edited of news and commercials. For a complete listing of over 600 interviews on cassette as well as selected videos and books, write to Laura Lee, P.O. Box 3010, Bellevue, Washington 98009, or call the hotline at 1-800-243-1438 for the newest listings